Have you ever felt like you were carrying around a little extra weight, but not the kind you’d find on a scale? The uncomfortable, sometimes even painful, experience of constipation can leave you feeling frustrated and searching for relief. As a nurse, understanding the complexities of constipation and developing a comprehensive care plan is crucial in providing effective support to your patients. This article delves into the intricacies of constipation, explores effective nursing interventions, and provides a downloadable PDF care plan you can use to help your patients find lasting comfort.

Image: www.vrogue.co
Constipation, a common ailment affecting people of all ages, is characterized by infrequent bowel movements, hard stools, and difficulty passing stool. The underlying causes can range from lifestyle factors like poor diet and dehydration to underlying medical conditions like irritable bowel syndrome (IBS) or even certain medications. Understanding the root cause of constipation is crucial in developing an effective nursing care plan to help your patients regain their digestive comfort.
Unraveling the Mystery of Constipation
Before we dive into the nursing interventions, let’s first get a better understanding of this often misunderstood condition. Constipation isn’t just about infrequent bowel movements; it’s about the overall struggle with stool passage. Think of it like a traffic jam in the digestive system, where the stool can get stuck along its journey.
Causes of Constipation
Numerous factors can contribute to constipation, and recognizing these causes is vital in developing a personalized care plan.
-
Lifestyle Factors:
- Diet: A diet lacking in fiber, which is essential for adding bulk to stool and promoting regular bowel movements, is a common culprit. Think of fiber as the “grease” that helps things move smoothly through the digestive system.
- Hydration: Inadequate fluid intake can lead to hard and dry stools, making it challenging to pass them.
- Lack of Physical Activity: Regular exercise helps stimulate bowel contractions and promotes healthy digestion.
- Ignoring the Urge: Suppressing the urge to defecate can lead to delayed bowel movements and increased constipation.
-
Medical Conditions:
- IBS: Irritable bowel syndrome is a chronic condition that affects the large intestine, often leading to constipation, diarrhea, or alternating bouts of both.
- Hypothyroidism: This condition, where the thyroid gland doesn’t produce enough hormones, can disrupt normal bowel function.
- Diabetes: Diabetic neuropathy can impact the nerves responsible for bowel control, leading to constipation.
- Medications: Certain medications, including painkillers, antidepressants, and iron supplements, can contribute to constipation as a side effect.
Assessing the Severity
The severity of constipation can vary greatly. From mild occasional discomfort to severe, persistent issues, accurately assessing the level of constipation your patients are experiencing is key to appropriate care.
- Mild Constipation: This usually involves infrequent bowel movements (less than three times a week) with manageable difficulty passing stool.
- Moderate Constipation: Characterized by infrequent bowel movements, hard stools, and straining during bowel movements, leading to discomfort and potentially even anal fissures.
- Severe Constipation: This involves significant difficulty passing stool, extreme straining, and possibly requiring assistance with bowel movements.
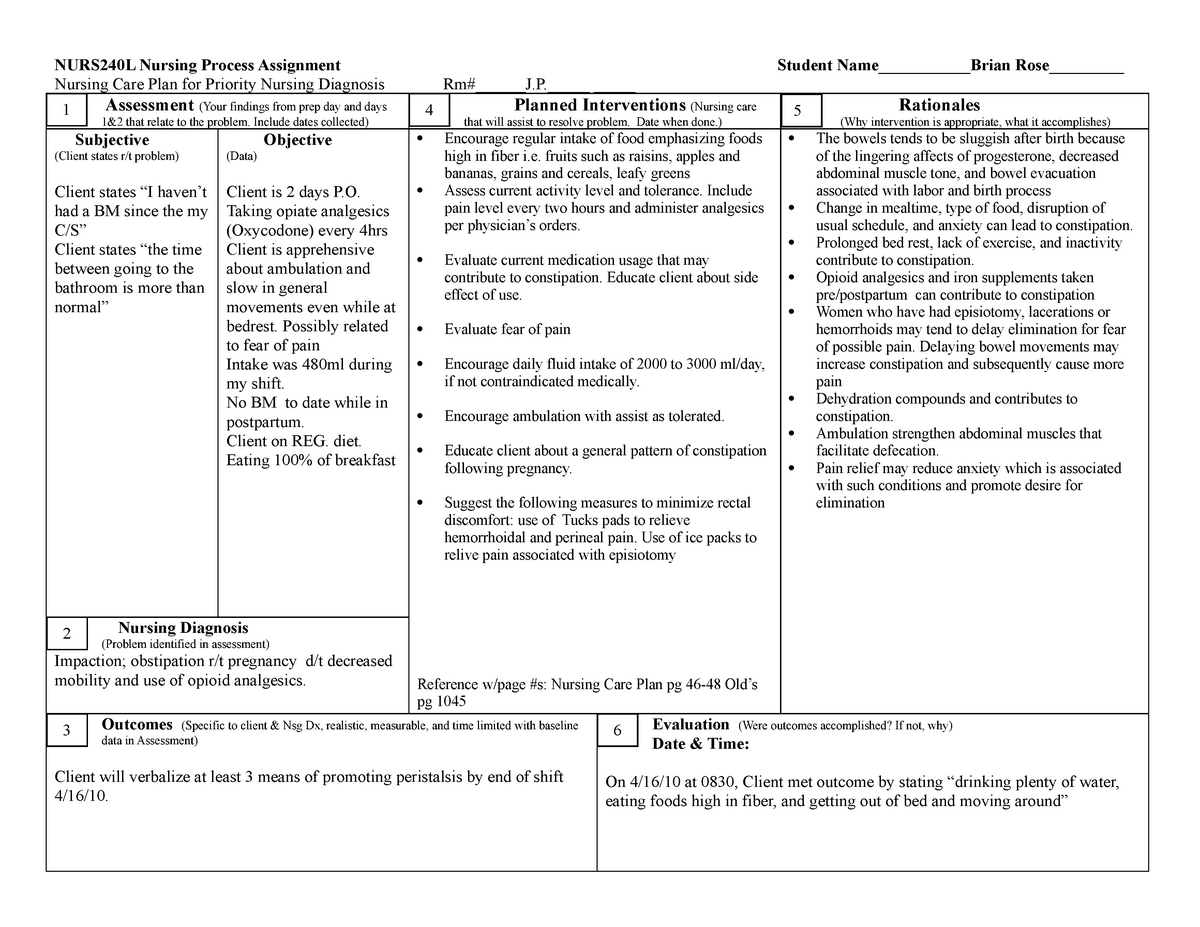
Image: www.aiophotoz.com
Analyzing the Impact of Constipation
It’s important to remember that constipation can have a profound impact on a patient’s well-being, extending beyond just digestive discomfort.
- Pain and Discomfort: Constipation can be intensely painful, with the straining and pressure during bowel movements causing discomfort and even anal fissures.
- Mental Health: The constant struggle with bowel movements can lead to feelings of frustration, anxiety, and even depression.
- Sleep Disturbances: The discomfort and pain associated with constipation can significantly disrupt sleep, impacting overall health and well-being.
- Social Implications: Dealing with constipation can significantly impact social activities and make it challenging to participate in everyday life.
Building a Solid Nursing Care Plan for Constipation
Now that we’ve explored the nuances of constipation, let’s discuss how to develop a comprehensive care plan that can effectively address this condition.
Initial Assessment: Gathering Key Information
A thorough assessment is the foundation of any successful care plan.
- Medical History: Inquire about any underlying medical conditions, including IBS, thyroid disorders, or diabetes, which could contribute to constipation.
- Medication History: Ask about any medications they’re taking, as certain drugs can cause constipation as a side effect.
- Dietary Habits: Explore their typical diet, including fiber intake, fluid consumption, and any recent changes in their eating patterns.
- Bowel Habits: Understand their normal bowel frequency, the consistency of their stools, and their experience with straining or discomfort during bowel movements.
- Lifestyle: Discuss their level of physical activity, sleep habits, and any potential stress triggers.
Developing a Personalized Plan
Based on your assessment, you can tailor a care plan that addresses your patient’s specific needs and circumstances.
Dietary Intervention
- High-Fiber Diet: Increasing fiber intake is crucial for promoting regular bowel movements. Encourage a daily intake of fruits, vegetables, and whole grains. You can recommend a high-fiber supplement for extra support.
- Fluid Intake: Ensure adequate fluid intake by encouraging your patients to drink plenty of water throughout the day. This is essential for softening stool and making it easier to pass.
Lifestyle Modifications
- Regular Exercise: Regular physical activity helps stimulate bowel contractions and promotes regular bowel movements. Recommend at least 30 minutes of moderate-intensity exercise most days of the week.
- Regular Bowel Habits: Encourage your patients to establish a consistent bowel routine by setting aside a specific time each day for defecation.
- Stress Management: Stress can contribute to constipation. Teach patients relaxation techniques such as deep breathing exercises, meditation, or yoga.
Pharmacological Interventions
- Stool Softeners (Lubricants): These medications work by adding moisture to stool and making it easier to pass.
- Bulk-Forming Laxatives: These fiber supplements are similar to dietary fiber, adding bulk to stools and promoting regularity.
- Stimulant Laxatives: These laxatives directly stimulate bowel contractions, encouraging bowel movements.
- Osmotic Laxatives: These medications draw water into the colon, softening stool and promoting defecation.
Other Considerations
- Rectal Stimulation: If other interventions are ineffective, rectal stimulation with a digital rectal examination or a rectal suppository might be necessary to trigger a bowel movement.
Monitoring and Evaluation
Once you’ve established a care plan, it’s crucial to monitor and evaluate its effectiveness.
- Bowel Frequency: Regularly monitor the frequency and consistency of their bowel movements.
- Stool Consistency: Assess the consistency of their stool, noting any changes in firmness or texture.
- Discomfort Level: Document any pain or discomfort they experience during bowel movements.
- Patient Education: Provide thorough education about the causes, management, and prevention of constipation.
Downloadable PDF Care Plan: Your Ultimate Guide
To make your life easier, we’ve developed a comprehensive nursing care plan for constipation in PDF format. This readily available resource provides you with a structured framework for developing individualized patient care plans.
The PDF includes:
- Assessment Guide: A comprehensive set of questions to guide your assessment process.
- Nursing Interventions: Detailed descriptions of various dietary, lifestyle, and pharmacological interventions.
- Evaluation Criteria: A set of factors to monitor and evaluate the effectiveness of your care plan.
- Patient Education Resources: A collection of links to reliable websites, pamphlets, and other materials that can educate your patients on constipation.
Nursing Care Plan For Constipation Pdf
Conclusion
Constipation, while often viewed as a minor inconvenience, can significantly impact a person’s overall well-being. As a nurse, you have a vital role in understanding the complexities of this condition, developing effective care plans, and providing your patients with the support and education they need to regain their digestive comfort and improve their quality of life.
This article has provided you with the tools and knowledge to build a solid foundation for your nursing care plans related to constipation. By understanding the underlying causes, employing evidence-based interventions, and monitoring your patients’ progress closely, you can empower them to manage this condition effectively and alleviate their discomfort.
We encourage you to download our comprehensive care plan PDF today and start using it to improve the lives of your patients.





