Imagine experiencing a burning sensation every time you use the bathroom, feeling an urgent need to urinate frequently, and even noticing a change in the color or smell of your urine. These are just some of the uncomfortable symptoms associated with a urinary tract infection (UTI), a common ailment that affects millions of people worldwide. But fear not, because with proper care and attention, UTIs can be effectively managed. This article delves into the intricacies of a nursing care plan for UTI, offering valuable insights for both healthcare professionals and individuals seeking to understand this condition better.
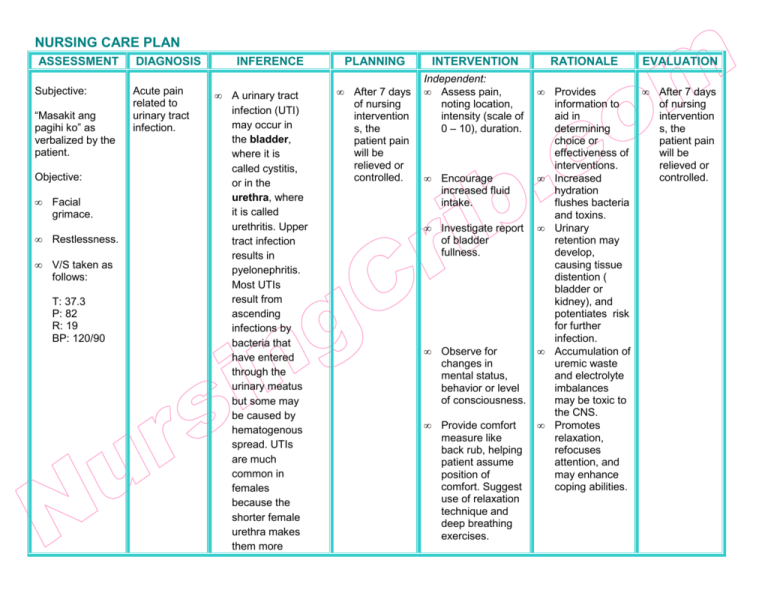
Image: www.aiophotoz.com
A UTI occurs when bacteria, usually from the gut, enter the urinary tract and multiply, causing inflammation and infection. While UTIs are typically treated with antibiotics, a comprehensive nursing care plan goes beyond medication to address the unique needs of each patient. From pain management and symptom relief to preventive measures and patient education, a well-structured care plan empowers individuals to regain their health and well-being.
Understanding the Pathophysiology and Predisposing Factors
Before delving into the nursing care plan, it’s essential to grasp the underlying factors that contribute to UTIs. The urinary tract, a complex system responsible for urine production and elimination, comprises the kidneys, ureters, bladder, and urethra. A UTI typically involves the lower urinary tract, encompassing the bladder and urethra, and less commonly, the upper urinary tract, involving the kidneys and ureters.
Several factors can predispose individuals to UTIs, including:
- Female anatomy: Women are more susceptible to UTIs due to the shorter urethra, making it easier for bacteria to travel from the anus to the bladder.
- Sexual activity: Engaging in sexual intercourse can increase the risk of UTIs, especially in women. It is recommended to urinate after sex to flush out any bacteria that may have entered the urethra.
- Menopause: After menopause, estrogen levels decline, affecting the vaginal flora and making women more vulnerable to UTIs.
- Catheterization: The use of catheters can increase the risk of UTIs, particularly in hospitalized patients.
- Diabetes: Individuals with diabetes are at a higher risk of UTIs due to impaired immune function.
- Kidney stones: The presence of kidney stones can obstruct urine flow, creating an environment conducive to bacterial growth.
- Weakened immune system: Individuals with suppressed immune systems, such as those undergoing chemotherapy or transplantation, are more prone to infections.
- Incomplete bladder emptying: Not emptying the bladder completely can allow bacteria to linger and multiply.
Assessment: Recognizing the Signs and Symptoms of UTI
A thorough assessment is the cornerstone of any nursing care plan for UTI, allowing healthcare providers to identify the presence of infection and tailor treatment accordingly. The assessment process typically involves:
- Patient history: Gathering information about the patient’s past medical history, including previous UTIs, diabetes, or other conditions that may increase their risk.
- Physical assessment: Assessing the patient’s vital signs, such as temperature, heart rate, blood pressure, and respiratory rate, to assess their overall health status.
- Genitourinary assessment: Exploring the patient’s urinary symptoms, including frequency, urgency, dysuria (painful urination), hematuria (blood in urine), and incontinence.
- Gastrointestinal assessment: Assessing the patient’s abdominal pain, nausea, vomiting, or other gastrointestinal symptoms, as UTIs can sometimes present with these complications.
- Neurological assessment: Assessing the patient’s mental status, including confusion or delirium, which can be a sign of a severe UTI or complications like sepsis.
Diagnostic Testing: Confirming the Diagnosis
Once the initial assessment is completed, diagnostic tests may be ordered to confirm the diagnosis of a UTI. These tests include:
- Urinalysis: A urinalysis examines the urine for the presence of white blood cells, red blood cells, bacteria, and nitrates. These findings can indicate an infection and help differentiate between UTIs and other conditions.
- Urine culture and sensitivity: A urine culture is a more definitive test that identifies the specific type of bacteria causing the infection. This information is crucial for determining the most effective antibiotic treatment.
- Imaging studies: In cases of suspected complications or upper urinary tract infections, imaging studies like ultrasound or CT scans may be used to visualize the urinary tract and identify any abnormalities.

Image: www.vrogue.co
Nursing Interventions: Providing Holistic Care
A comprehensive nursing care plan for UTI focuses on managing symptoms, promoting healing, and preventing recurrence. The key interventions include:
Pain Management
UTIs can cause significant discomfort, particularly during urination. Pain management is an essential aspect of care. Nursing interventions include:
- Analgesics: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can provide temporary relief from pain and inflammation.
- Heat therapy: Applying a warm compress to the lower abdomen or back can help soothe discomfort and relax muscles.
- Sitz baths: Warm sitz baths can provide comfort and promote healing by reducing inflammation and promoting blood flow to the pelvic region.
Fluid Management
Hydration is crucial for flushing out bacteria and relieving urinary symptoms. Encourage the patient to drink plenty of fluids, aiming for at least eight glasses of water per day. Avoid caffeine and alcohol, which can exacerbate urinary urgency and frequency.
Symptom Relief
Nursing interventions are aimed at minimizing the impact of UTI symptoms on the patient’s quality of life:
- Urinary frequency and urgency: Educate the patient about the importance of frequent urination to empty the bladder completely. Encourage them to avoid caffeine and alcohol, which can irritate the bladder.
- Dysuria: Provide pain relief measures as mentioned previously, such as analgesics and sitz baths. Encourage the patient to urinate in warm water to reduce burning sensations.
- Hematuria: If blood is present in the urine, monitor the patient for any signs of worsening symptoms or complications. Encourage adequate hydration to promote urine flow and help flush out the blood cells.
Antibiotic Therapy
Antibiotics are the mainstay of treatment for UTIs. Nurses play a crucial role in administering antibiotics accurately and monitoring for any side effects. Educate the patient about the importance of completing the entire course of antibiotics, even if symptoms improve, to prevent bacterial resistance.
Preventing Recurrence
A key component of nursing care is educating patients about preventive measures to reduce the risk of recurrent UTIs:
- Hygiene practices: Encourage frequent handwashing, especially before and after using the bathroom. Explain the importance of wiping from front to back to prevent bacterial contamination.
- Hydration: Remind patients to drink ample fluids throughout the day, as this helps flush out bacteria from the urinary tract.
- Urinary habits: Teach patients to empty their bladder completely each time they urinate. Avoid straining or holding urine for long periods.
- Sexual practices: Encourage women to urinate immediately after sexual intercourse to flush out any bacteria that may have entered the urethra.
Patient Education
Nurses play a critical role in educating patients about UTIs and how to manage their condition effectively. Provide clear and concise information about:
- Signs and symptoms: Explain the common symptoms of UTIs, encouraging patients to seek medical attention if they experience any concerning symptoms.
- Risk factors: Discuss the factors that increase the risk of UTIs, such as female anatomy, sexual activity, and diabetes.
- Treatment options: Explain the role of antibiotics in treating UTIs and the importance of completing the entire course of medication.
- Preventive measures: Educate patients about hygiene practices, fluid intake, and urinary habits to reduce the risk of future UTIs.
- Follow-up care: Emphasize the importance of follow-up appointments to monitor the effectiveness of treatment and discuss any lingering concerns.
Nursing Care Plan For Uti Urinary Tract Infection
Conclusion
A nursing care plan for UTI is a comprehensive approach that addresses various aspects of the patient’s needs, from pain management to symptom relief and education. By providing individualized care and empowering patients with knowledge about their condition, nurses play a vital role in promoting optimal health outcomes for individuals with UTIs. It’s crucial to remember that UTIs are treatable, and with proper care, individuals can regain their well-being and live fulfilling lives. Continue to seek guidance from healthcare professionals for any concerns or questions you may have about UTIs or other health conditions.





