Imagine this: You’re a nurse taking care of a patient recovering from a stroke. Their swallowing ability is compromised, making them vulnerable to aspiration – a frightening situation where food or liquid enters the airway instead of the stomach. This can lead to serious complications like pneumonia. This is just one example of why understanding and implementing a nursing care plan for aspiration risk is crucial. With a comprehensive plan, we can minimize the risk of this dangerous event and promote patient safety.
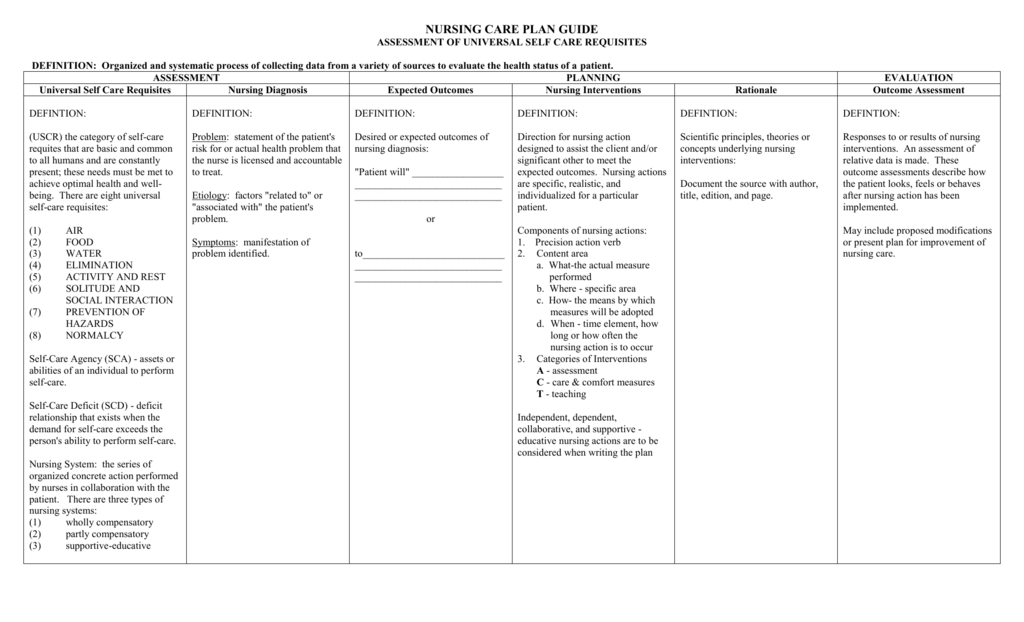
Image: nandanursing.blogspot.com
This article will delve into the complexities of aspiration risk, exploring the causes, consequences, and strategies for prevention. We will also provide a detailed framework for developing a comprehensive nursing care plan tailored to each patient’s individual needs. Whether you’re a seasoned nurse or a curious reader wanting to learn more about this important topic, join us as we uncover the essential information to provide optimal care for those at risk of aspiration.
Understanding Aspiration Risk
What is Aspiration?
Aspiration is the unintentional entry of food, liquid, or other substances into the airway, bypassing the esophagus and reaching the lungs. This can happen during swallowing, vomiting, or even during routine activities like talking or coughing. When foreign substances enter the lungs, they can cause inflammation, infection, and even permanent lung damage.
Who is at Risk of Aspiration?
Certain individuals are more susceptible to aspiration than others. These include:
- Patients with neurological conditions: Strokes, brain injuries, and dementia can impair swallowing reflexes and coordination.
- Patients with neuromuscular disorders: Conditions like amyotrophic lateral sclerosis (ALS) and muscular dystrophy weaken the muscles involved in swallowing, increasing risk.
- Patients with head and neck cancers: Surgical interventions or radiation therapy can affect swallowing ability.
- Patients with gastrointestinal conditions: Gastroesophageal reflux disease (GERD) and hiatal hernias can lead to frequent reflux, increasing the risk of aspiration.
- Individuals with weakened immune systems: Compromised immune systems make individuals more vulnerable to infections following aspiration.
- Individuals with a history of aspiration: Previous aspiration episodes can increase the risk of future occurrences.

Image: www.scribd.com
Developing a Nursing Care Plan for Aspiration Risk
Assessment and Evaluation
Before creating a care plan, a thorough assessment is essential. This includes:
- Reviewing medical history: Documenting any predisposing conditions, previous aspiration experiences, and current medications.
- Evaluating swallowing function: Observing the patient’s ability to swallow different textures, identifying any signs of aspiration like coughing or choking.
- Assessing neurological status: Checking for alertness, cognitive function, and any neurological impairments affecting swallowing.
- Monitoring vital signs: Observing temperature, heart rate, and respiratory rate for any signs of infection or distress.
Care Plan Development
Once the assessment is complete, a tailored care plan should be developed, incorporating the following strategies:
Positioning
- High Fowler’s position: Elevating the head of the bed to 60-90 degrees during meals and for at least 2 hours after eating.
- Head-of-bed elevation during sleep: Using pillows to elevate the head to at least 30 degrees even during sleep.
Dietary Modifications
- Thickened liquids: Thicken liquids like water, juice, and soups to improve viscosity and slow down swallowing.
- Pureed foods: Offer pureed foods, avoiding solid foods that are difficult to manipulate and swallow.
- Smaller meal portions: Divide meals into smaller, more manageable portions.
- Avoiding certain foods: Discourage foods that are sticky, crumbly, or prone to sticking in the throat.
Swallowing Techniques
- Chin tuck technique: Encourage chin tuck while swallowing to help close the airway.
- Head tilt technique: Tilt the head slightly forward while swallowing to facilitate food traveling down the esophagus.
- Multiple swallows: Promote multiple swallows to ensure the complete passage of food.
- Slow pace: Encourage patients to eat slowly and savor each bite.
Environmental Support
- Quiet and distraction-free environment: Minimize distractions and create a calm atmosphere during meals.
- Proper lighting: Ensure adequate lighting to enhance visibility and facilitate mealtime.
- Comfortable seating: Provide a comfortable and supportive chair to promote good posture.
Oral Hygiene
- Frequent oral care: Encourage regular brushing and flossing to prevent food accumulation and bacteria in the mouth.
- Dental check-ups: Ensure regular dental check-ups to address any potential dental issues that can affect swallowing.
Medication Management
- Medication review: Review medications for any that might affect swallowing or cause dry mouth.
- Administering medications: Use appropriate techniques for administering medications, such as crushing tablets or ensuring adequate fluid intake alongside medication.
Collaboration with Speech-Language Pathologist
Close collaboration with a speech-language pathologist (SLP) is crucial. An SLP can perform a thorough swallowing evaluation, identify specific swallowing difficulties, and suggest strategies for improvement. They can also provide training on swallowing techniques and recommend appropriate food textures and consistencies.
Latest Trends and Developments
Technology is continually evolving to aid in aspiration prevention. Innovations like videofluoroscopic swallowing studies (VFSS) allow for real-time visualization of the swallowing process, enabling clinicians to assess swallowing function and identify any aspiration risks.
Furthermore, research is ongoing to develop new therapeutic approaches to improve swallowing function in patients with neurological disorders. This includes exploring the use of electrical stimulation to enhance muscle activity and facilitate swallowing.
Tips and Expert Advice from a Nurse
Listen to Patients
Every patient is different. Pay close attention to a patient’s self-reported concerns about swallowing difficulties. If they express difficulty swallowing a specific food, respect their feedback. Remember, providing reassurance and emotional support is crucial when a patient feels vulnerable.
Observe Swallowing Behavior
Carefully observe a patient’s swallowing behavior. Look for signs of aspiration like choking, coughing, or gagging after swallowing. Assess for any changes in voice quality, such as hoarseness, as it could indicate aspiration.
Patient Education
Empowering patients to become active participants in their own care is essential. Involve them in decision-making regarding their diet, swallowing techniques, and medication management.
Frequently Asked Questions (FAQs)
Q1: What are the signs and symptoms of aspiration?
Signs of aspiration include coughing, choking, gagging, wheezing, or having a wet or gurgling voice. Fever, shortness of breath, and chest pain can also signify a possible aspiration event.
Q2: What are the risks of aspiration?
Aspiration can cause pneumonia, lung infections, and even permanent lung damage. If aspiration occurs repeatedly, the risk of these complications increases. Aspiration can also lead to respiratory failure and complications related to nutritional status.
Q3: Are there any medications to prevent aspiration?
While there isn’t a specific medication to prevent aspiration, treating underlying conditions such as GERD through medication can reduce the risk. Additionally, anti-anxiety medications can sometimes be helpful to reduce anxiety-related swallowing difficulties.
Nursing Care Plan For Risk Of Aspiration
Conclusion
A comprehensive nursing care plan for aspiration risk is essential to ensure patient safety and prevent potential complications. It involves a thorough assessment of the patient’s individual needs, customized interventions to address swallowing difficulties, and ongoing monitoring to identify and manage any emerging issues. Remember, collaboration with other healthcare professionals, especially speech-language pathologists, is crucial for optimal care.
Do you have any personal experiences with aspiration or any questions about this topic? Share your thoughts below!





