Imagine a patient struggling to breathe, their chest heaving with each labored breath. The air they gasp for feels scarce, making every effort to inhale a monumental challenge. This is the reality of ineffective airway clearance, a common nursing concern that requires immediate attention and a well-crafted care plan. Nurses play a vital role in assessing the situation, implementing interventions, and monitoring the patient’s progress toward regaining effective airway clearance.
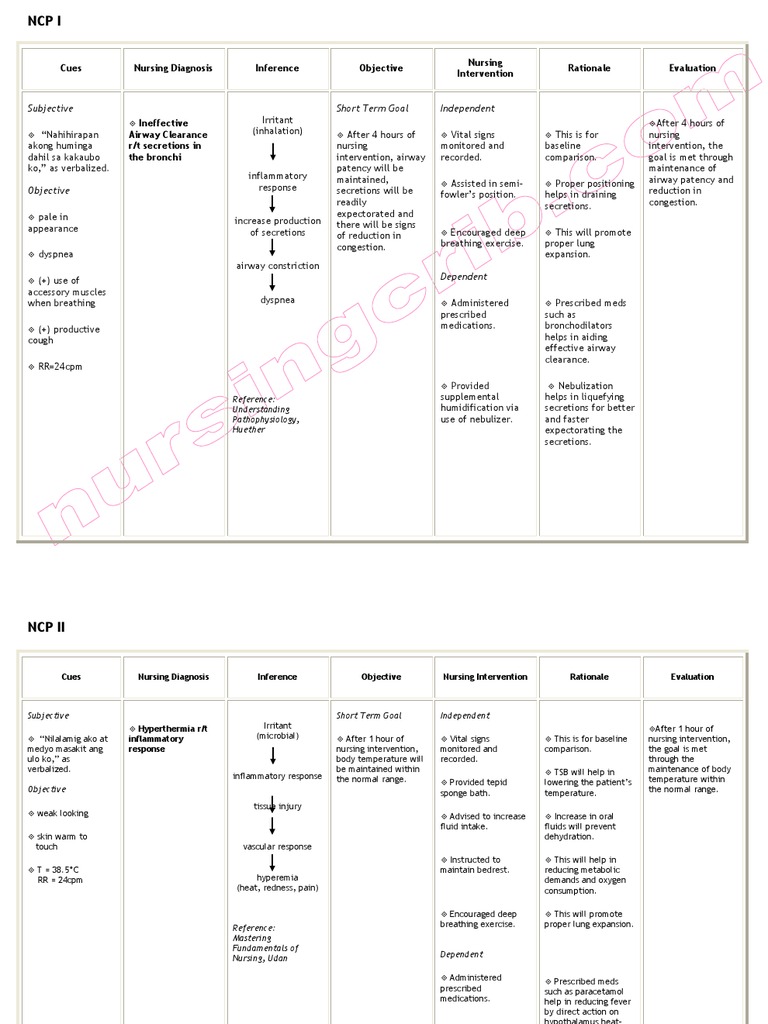
Image: www.scribd.com
While every patient is unique, the foundation of a successful care plan revolves around a thorough understanding of the underlying cause, accurate symptom identification, and timely interventions. This article will delve into the intricacies of crafting a comprehensive nursing care plan for ineffective airway clearance, providing insights into challenges, interventions, and evaluation strategies.
Understanding Ineffective Airway Clearance
Defining the Problem
Ineffective airway clearance is a nursing diagnosis that describes a patient’s inability to effectively remove secretions from their airway. These secretions, whether mucus, phlegm, or foreign objects, can obstruct airflow, leading to breathing difficulties, increased risk of infection, and compromised oxygenation. This condition can affect individuals of all ages and can stem from a wide array of factors, including underlying medical conditions, environmental factors, and even medications.
Causes of Ineffective Airway Clearance
The causes of ineffective airway clearance are diverse and often interconnected. Common culprits include:
- Respiratory Conditions: Chronic obstructive pulmonary disease (COPD), pneumonia, asthma, cystic fibrosis, and bronchiectasis can contribute to excessive mucus production and airway narrowing, making it difficult to clear secretions.
- Neuromuscular Disorders: Conditions like multiple sclerosis, amyotrophic lateral sclerosis (ALS), and spinal cord injuries can impair muscle control, making it difficult to cough effectively and clear the airway.
- Traumatic Injuries: Head injuries, chest trauma, and surgical procedures can cause airway obstruction by damaging tissues or causing inflammation.
- Post-Surgical Complications: Following surgery, especially on the chest or upper respiratory tract, swelling and pain can interfere with effective airway clearance.
- Medications: Certain medications, like sedatives or opioid pain relievers, can suppress the cough reflex, increasing the risk of airway obstruction.
- Environmental Factors: Exposure to pollutants, smoke, dust, and allergens can irritate the airways, trigger mucus production, and make it harder to clear secretions.
Image: athleattoathlete.blogspot.com
Symptoms of Ineffective Airway Clearance
Recognizing the signs of ineffective airway clearance is crucial for timely intervention. Common symptoms include:
- Dyspnea: Difficulty breathing, shortness of breath, and wheezing.
- Cough: Persistent cough, often producing thick mucus or phlegm.
- Wheezing: A high-pitched whistling sound during exhalation, indicating airway narrowing.
- Rales or Crackles: Abnormal crackling or bubbling sounds in the lungs, suggesting fluid buildup in the airways.
- Cyanosis: Bluish discoloration of the skin or lips, indicating low oxygen levels in the blood.
- Increased Respiratory Rate: Rapid breathing as the body tries to compensate for low oxygen levels.
- Fatigue: Persistent weakness and tiredness due to the effort required to breathe.
- Chest Discomfort: Tightness, pressure, or pain in the chest.
Developing a Nursing Care Plan for Ineffective Airway Clearance
A well-structured nursing care plan for ineffective airway clearance serves as a roadmap for providing optimal care to patients struggling with this condition. It guides nurses in assessing the patient’s needs, implementing interventions, and monitoring their progress.
Assessment: The Foundation of Care
The assessment process is paramount in developing an effective care plan. It involves gathering comprehensive information about the patient’s condition, including:
- History: The patient’s medical history, including previous respiratory illnesses, surgeries, and medications.
- Physical Examination: Observing the patient’s breathing pattern, auscultating lung sounds, and assessing their respiratory rate, pulse, and oxygen saturation.
- Secretion Characteristics: Observing the color, consistency, and amount of secretions produced by the patient.
- Cough Effectiveness: Assessing the patient’s ability to cough productively and clear their airway effectively.
- Patient’s Perception: Listening to the patient’s description of their symptoms, their level of discomfort, and their ability to manage their breathing.
Diagnosing Ineffective Airway Clearance
Once the assessment is complete, nurses use their clinical judgment to formulate a nursing diagnosis reflecting the patient’s condition. In this case, the likely nursing diagnosis would be “Ineffective Airway Clearance” with specific defining characteristics, such as:
- Difficult or labored breathing
- Coughing with or without productive sputum
- Wheezing or other abnormal breath sounds
- Decreased oxygen saturation levels
- Cyanosis (blue tint to skin)
- Increased respiratory rate
- Anxiety or restlessness
Planning: Setting Goals and Interventions
The planning phase of the care plan involves setting realistic and measurable goals for the patient and outlining interventions to help achieve those goals. Common goals include:
- Improved Breath Sounds: Clear and audible breath sounds with minimal or no wheezing or crackles.
- Effective Coughing: The patient demonstrating the ability to cough productively and expel airway secretions.
- Clear Airway: The patient exhibiting clear and unobstructed airways, allowing for adequate oxygenation and ventilation.
- Increased Oxygen Saturation: Achieving and maintaining a stable and acceptable oxygen saturation level.
- Reduced Respiratory Distress: The patient experiencing decreased shortness of breath and improved breathing effort.
- Increased Activity Tolerance: The patient able to participate in activities of daily living without significant respiratory distress.
Interventions are the actions taken to achieve these goals. The most common interventions for ineffective airway clearance include:
- Hydration: Encourage patients to drink plenty of fluids to thin mucus secretions, making them easier to clear.
- Humidification: Use a humidifier to add moisture to the air, which can help loosen secretions and improve airflow.
- Positioning: Place the patient in a semi-Fowler’s or high Fowler’s position to promote lung expansion and drainage.
- Chest Physiotherapy: Techniques like postural drainage, percussion, and vibration can help mobilize secretions and improve airway clearance.
- Effective Coughing: Teach patients deep breathing exercises and coughing techniques to effectively clear their airways.
- Suctioning: Use a suction catheter to remove secretions that cannot be cleared through coughing.
- Oxygen Therapy: Provide supplemental oxygen as needed to improve oxygenation and alleviate respiratory distress.
- Medications: Administer bronchodilators to open airways and mucolytics to thin mucus.
Implementation: Putting the Plan into Action
Implementing the care plan involves actively applying the chosen interventions and monitoring the patient’s response. This includes:
- Encouraging Fluid Intake: Providing fluids regularly and ensuring the patient is hydrated.
- Assisting with Positioning: Helping the patient change positions frequently to promote drainage.
- Administering Medications: Giving prescribed medications on time and following protocols.
- Providing Chest Physiotherapy: Implementing chest physiotherapy techniques as prescribed.
- Suctioning When Necessary: Using suctioning techniques to remove secretions when coughing is ineffective.
- Monitoring Oxygen Levels: Regularly checking oxygen saturation levels and adjusting oxygen delivery as needed.
Evaluation: Tracking Progress and Making Adjustments
The evaluation phase is critical to determine the effectiveness of the care plan and make adjustments as needed. This includes:
- Monitoring Vital Signs: Observing changes in respiratory rate, pulse, blood pressure, and oxygen saturation.
- Assessing Breath Sounds: Listening to lung sounds to evaluate the effectiveness of interventions.
- Evaluating Cough Effectiveness: Assessing the patient’s ability to cough productively and clear airway secretions.
- Monitoring Secretion Characteristics: Observing the color, consistency, and amount of secretions produced.
- Observing Patient Comfort: Assessing the patient’s level of discomfort and ability to breathe comfortably.
- Re-evaluating Goals: Reviewing the established goals and making adjustments as necessary based on the patient’s progress.
Evaluation is an ongoing process. By regularly monitoring the patient’s response to interventions, nurses can identify areas where the care plan needs modification to better address the patient’s needs.
Trends and Developments in Ineffective Airway Clearance Management
The field of respiratory care is constantly evolving, with new advancements in technology, medication, and treatment approaches emerging regularly. Some noteworthy trends include:
- High-Frequency Oscillatory Ventilation (HFOV): This technique is used for patients with severe respiratory distress, especially those with chronic lung disease. HFOV delivers rapid, small-volume breaths to improve oxygenation and ventilation.
- Non-Invasive Ventilation (NIV): This approach utilizes masks or helmets to deliver pressurized air to the patient without the need for intubation.
- Smart Inhalers: New inhalers incorporate features like digital sensors that track usage, remind patients to take their medications, and provide real-time data to healthcare providers.
- Airway Clearance Devices: A range of devices, including vibrating vests and airway clearance systems, are being developed to help patients with airway clearance.
- Personalized Medicine: Advances in genomics and personalized medicine allow for tailoring interventions, including medications, to individual patients’ genetic predispositions and disease characteristics.
Expert Advice: Tips for Effective Care
From my experience as a nurse, here are some key tips to ensure the best possible care for patients with ineffective airway clearance:
- Communication is Key: Clear and consistent communication with the patient, their family, and other healthcare professionals is vital. This fosters understanding, collaboration, and a sense of shared responsibility for the patient’s care.
- Individualize Patient Care: Remember that every patient is unique. Tailor the care plan to the individual’s needs, incorporating their preferences and any relevant cultural considerations.
- Be Patient and Empathetic: Ineffective airway clearance can be a frustrating and distressing condition for patients. Be patient and empathetic as you support them through their challenges.
- Educate the Patient: Educate patients about their condition, treatment options, and how they can be actively involved in their care.
- Utilize Evidence-Based Practices: Stay up-to-date on the latest evidence-based practices and incorporate them into your care plan.
- Collaborate with Other Professionals: Work closely with respiratory therapists, physicians, and other members of the healthcare team to provide coordinated and holistic care.
By following these tips, nurses can provide effective, compassionate, and patient-centered care to individuals struggling with ineffective airway clearance, helping them regain optimal respiratory function.
Frequently Asked Questions (FAQs)
Q: What are some common complications associated with ineffective airway clearance?
A: Complications can include:
- Pneumonia: Secretions can accumulate in the lungs, creating an environment for bacteria to grow and potentially lead to pneumonia.
- Respiratory Failure: If the airway obstruction is severe, patients may experience respiratory failure, requiring assisted breathing through a ventilator.
- Hypoxemia: Low blood oxygen levels can lead to hypoxemia, potentially resulting in organ damage and other complications.
Q: How long does it typically take to improve airway clearance?
A: The duration of treatment varies considerably depending on the underlying cause, severity of the condition, and individual patient factors. It could take days, weeks, or even months to achieve significant improvement.
Q: What are some long-term strategies to prevent ineffective airway clearance?
A: Long-term strategies include:
- Managing underlying conditions: Address any underlying medical conditions that contribute to ineffective airway clearance.
- Maintaining a healthy lifestyle: Engaging in regular exercise, maintaining a healthy weight, and eating a balanced diet can help improve lung function and overall health.
- Avoiding irritants: Limit exposure to smoke, pollution, dust, and other environmental irritants.
- Handwashing: Practice good hygiene to reduce the risk of respiratory infections.
Nursing Care Plan Ineffective Airway Clearance
Conclusion
Managing ineffective airway clearance is a crucial aspect of nursing care. By understanding the underlying causes, employing a structured assessment and care plan, and implementing evidence-based interventions, nurses can play a vital role in helping patients regain effective airway clearance, improve their quality of life, and prevent serious complications. This article has provided a thorough overview of this nursing diagnosis, highlighting essential assessment, planning, implementation, and evaluation strategies to guide nurses in providing exceptional care. Are you interested in learning more about specific techniques or interventions related to ineffective airway clearance? Let us know in the comments below!





