Imagine a patient arriving at the emergency room with sudden weakness on one side of their body, slurred speech, and confusion. The clock is ticking, and every minute counts. How do medical professionals determine the severity of the stroke and initiate the appropriate treatment? Enter the National Institutes of Health (NIH) Stroke Scale, a crucial tool for rapid, standardized assessment of stroke patients.

Image: helihuhtala.blogspot.com
The NIH Stroke Scale is a critical component of stroke care globally. It allows medical professionals to objectively evaluate a patient’s neurological function, guiding them to make informed decisions about treatment and prognosis. In the midst of a medical emergency, the NIH Stroke Scale empowers healthcare providers to streamline patient care and potentially improve outcomes. Understanding its components, including the intricacies of Group A, becomes essential for anyone involved in stroke care, from nurses to physicians to paramedics.
What is the NIH Stroke Scale and Why is it Important?
The NIH Stroke Scale, often referred to as the NIHSS, is a 15-item neurological examination used to assess stroke severity. It was developed in the 1980s and has become the gold standard for evaluating stroke patients in acute care settings. The NIHSS is a structured tool that helps doctors consistently evaluate a patient’s neurological function, specifically focusing on aspects like:
- Level of Consciousness: Assessing the patient’s alertness and responsiveness.
- Eye Movements: Examining how well the patient can move their eyes and follow instructions.
- Visual Fields: Determining if the patient has any blind spots.
- Motor Function: Evaluating the strength and coordination of the patient’s limbs.
- Sensory Function: Testing the patient’s ability to feel touch, pain, and temperature.
- Language: Assessing the clarity and fluency of speech.
- Attention & Neglect: Observing the patient’s ability to focus and whether they are ignoring one side of their body.
Each item on the NIH Stroke Scale is assigned a score ranging from 0 to 4, with higher scores indicating more severe neurological deficits. The total score, ranging from 0 to 42, provides a comprehensive picture of the patient’s neurological status. This scoring system helps to:
- Objectively quantify stroke severity: Doctors can compare scores over time to track progress or identify deterioration.
- Guide treatment decisions: The NIHSS score helps determine eligibility for treatments like tissue plasminogen activator (tPA), a clot-busting drug.
- Predict patient outcomes: A higher NIHSS score is often associated with poorer outcomes, like longer hospital stays and increased disability.
- Facilitate communication among healthcare professionals: Everyone involved in the patient’s care, from nurses to physical therapists, understands the standardized language of the NIHSS.
Understanding Group A on the NIH Stroke Scale
The NIH Stroke Scale is divided into six different groups: Group A, B, C, D, E, and F. Each group focuses on specific neurological functions. Group A, specifically, delves into the assessment of the patient’s level of consciousness. This group holds significant importance as it gauges the patient’s responsiveness and awareness, offering crucial insights into the severity of the stroke and its impact on vital functions.
The Items in Group A: Unraveling the Mysteries of Consciousness
Group A of the NIH Stroke Scale consists of two items:
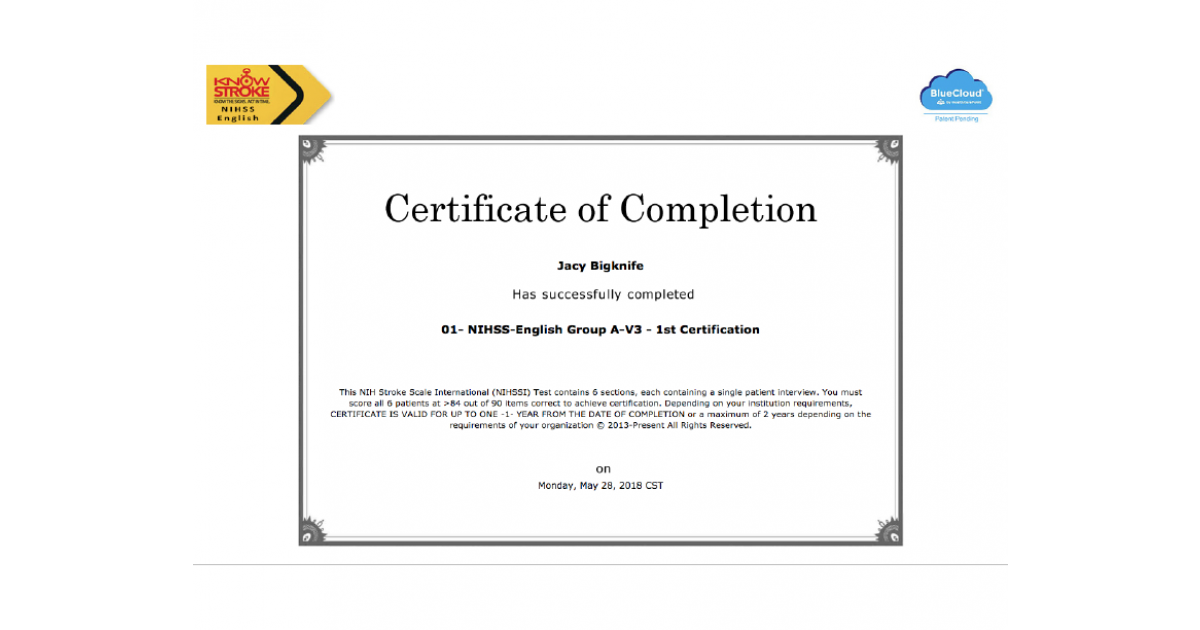
Image: portfolium.com
Item 1a: Level of Consciousness
This item tests the patient’s alertness and responsiveness. The examiner observes the patient and scores them based on their response to three simple commands:
- 0 points: The patient is alert and fully oriented.
- 1 point: The patient is drowsy but can be aroused by a simple command or light touch.
- 2 points: The patient is lethargic and requires repeated stimulation to arouse.
- 3 points: The patient is comatose and does not respond to any stimuli.
Item 1b: Best Motor Response
This item assesses the patient’s motor function, particularly their ability to follow commands and move their limbs. The examiner observes the patient’s response to three different commands:
- 0 points: The patient can follow commands, showing normal motor function.
- 1 point: The patient can follow simple commands, but their motor function is reduced.
- 2 points: The patient only responds to painful stimuli or shows localized withdrawal to pain.
- 3 points: The patient has decorticate posturing, a specific type of abnormal response to pain (rigidly extended legs and flexed arms with clenched fists).
- 4 points: The patient has decerebrate posturing another type of abnormal response to pain (rigidly extended limbs, including arms, with extended arms).
Interpreting Group A Results: Deciphering the Clues
The scores from Group A provide essential insights into the patient’s overall neurological status. A score of 0 on both items 1a and 1b indicates full alertness and normal motor responses, suggesting a less severe stroke or possibly a non-stroke event. However, as scores increase on either item, the severity of the neurological compromise grows.
For instance, a score of 3 on Item 1a signifies that the patient is comatose, suggesting a significant stroke affecting the brain’s ability to regulate consciousness. This score signals a critical neurological event requiring immediate advanced medical care. Similarly, a score of 4 on Item 1b indicating decerebrate posturing, represents a grave neurological deficit, often associated with a large and damaging stroke.
The Significance of Group A in Stroke Certification
For those interested in pursuing stroke certification, understanding Group A is essential. Mastering the evaluation of level of consciousness and motor responses is crucial for accurately assessing stroke patients, making informed treatment decisions, and predicting patient outcomes. Moreover, the ability to effectively explain and document Group A scores during certification examinations demonstrates a solid understanding of the NIH Stroke Scale and its clinical implications.
The Future of Stroke Assessment: Embracing Innovation
While the NIH Stroke Scale remains a crucial cornerstone of stroke care, the field of stroke assessment continues to evolve. New technologies and methods, such as telemedicine and AI-powered imaging analysis, are emerging, offering potential to streamline and enhance stroke evaluation. Exploring these advancements remains vital for all healthcare professionals involved in stroke care.
Nih Stroke Scale Certification Answers Group A
Conclusion
The NIH Stroke Scale, especially its Group A component, is a critical tool for discerning the severity of a stroke and guiding patient care. Through this article, we have delved into the intricacies of this assessment, providing essential insights that empower healthcare professionals to confidently evaluate stroke patients and make informed decisions. As we navigate the ever-evolving landscape of stroke care, understanding the NIH Stroke Scale remains a cornerstone of responsible practice, contributing to the pursuit of effective and timely treatment that can make a real difference in the lives of stroke patients.





