Imagine this scenario: you’re caring for a patient, perhaps an elderly individual or someone recovering from surgery, and you notice they’re experiencing symptoms like a rapid heartbeat, dry mouth, and confusion. These could be signs of dehydration, a serious condition that can quickly escalate if left untreated. As nurses, we are trained to recognize these signs and proactively address the risk of fluid volume deficit. The goal is to prevent dehydration before it becomes a significant problem for our patients.
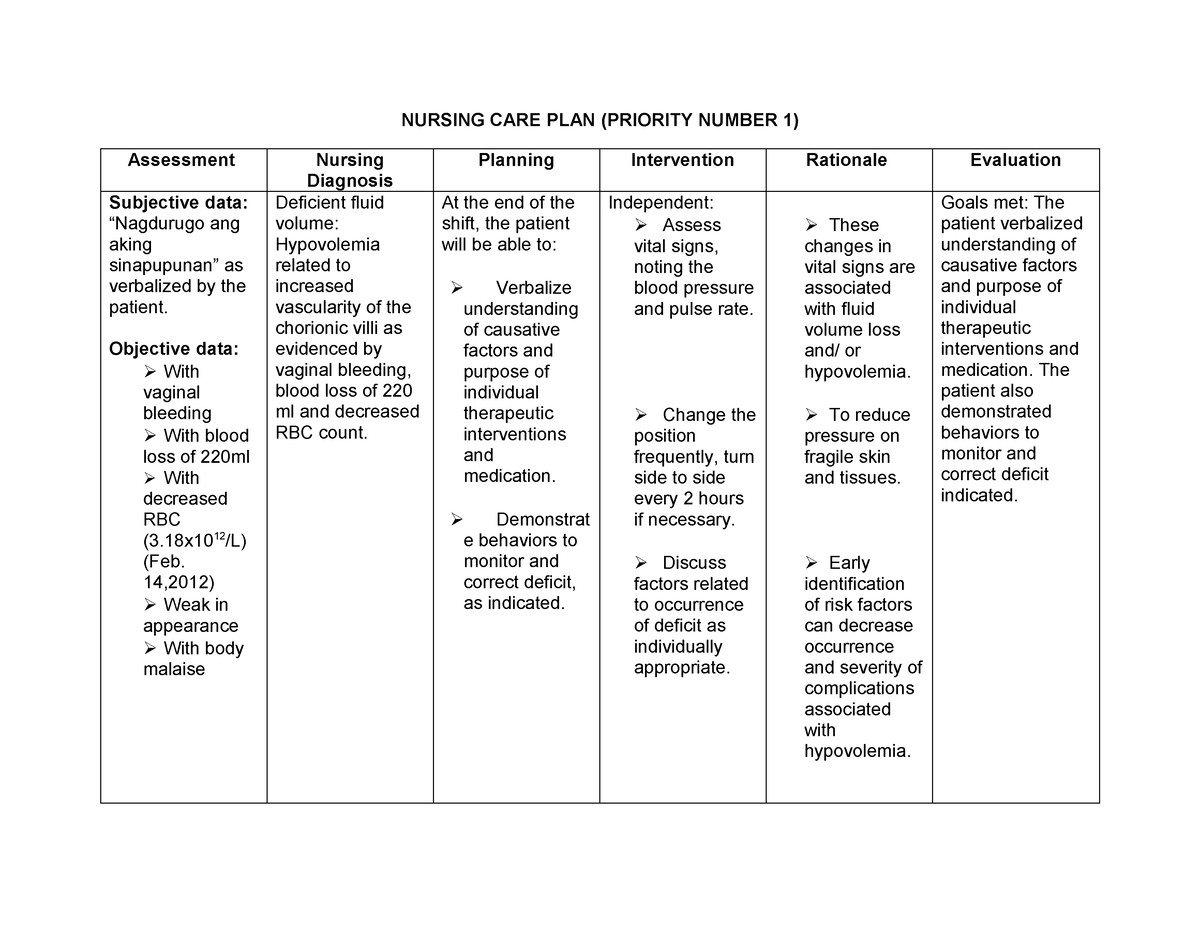
Image: www.sexizpix.com
This is where a comprehensive nursing care plan comes in. By implementing specific interventions and monitoring our patients closely, we can effectively manage the risk of fluid volume deficit. This article will delve into the world of nursing care plans, exploring the importance of recognizing risk factors, implementing effective interventions, and evaluating the effectiveness of our care.
Understanding Fluid Volume Deficit
Fluid volume deficit, often referred to as dehydration, occurs when the body loses more fluid than it takes in. This imbalance can lead to a range of problems, from mild discomfort to life-threatening complications. It’s crucial for nurses to be aware of the factors that contribute to fluid volume deficit and to have a solid understanding of how to assess, monitor, and manage this condition effectively.
There are many potential causes of fluid volume deficit, including:
Causes of Fluid Volume Deficit
- Inadequate Fluid Intake: This can be due to various reasons, including difficulty swallowing, lack of access to fluids, or simply forgetting to drink.
- Excessive Fluid Loss: This can occur through various routes:
- Gastrointestinal Tract: Vomiting, diarrhea, and excessive sweating can lead to significant fluid loss.
- Urine: Diuretics, diabetes, and kidney problems can increase urine production.
- Skin: Burns, wounds, and open skin can lead to fluid loss through evaporation.
Assessing Risk for Fluid Volume Deficit
The first step in managing fluid volume deficit is to accurately assess the patient’s risk. This involves gathering information about their medical history, current medications, and lifestyle. Nurses must carefully observe the patient for signs and symptoms of dehydration, including:
- Physical Signs:
- Tachycardia (rapid heartbeat)
- Hypotension (low blood pressure)
- Dry mucous membranes (mouth, tongue, eyes)
- Decreased skin turgor (skin elasticity)
- Sunken eyes
- Oliguria (decreased urine output)
- Mental Status: Confusion, lethargy, and dizziness can indicate dehydration.
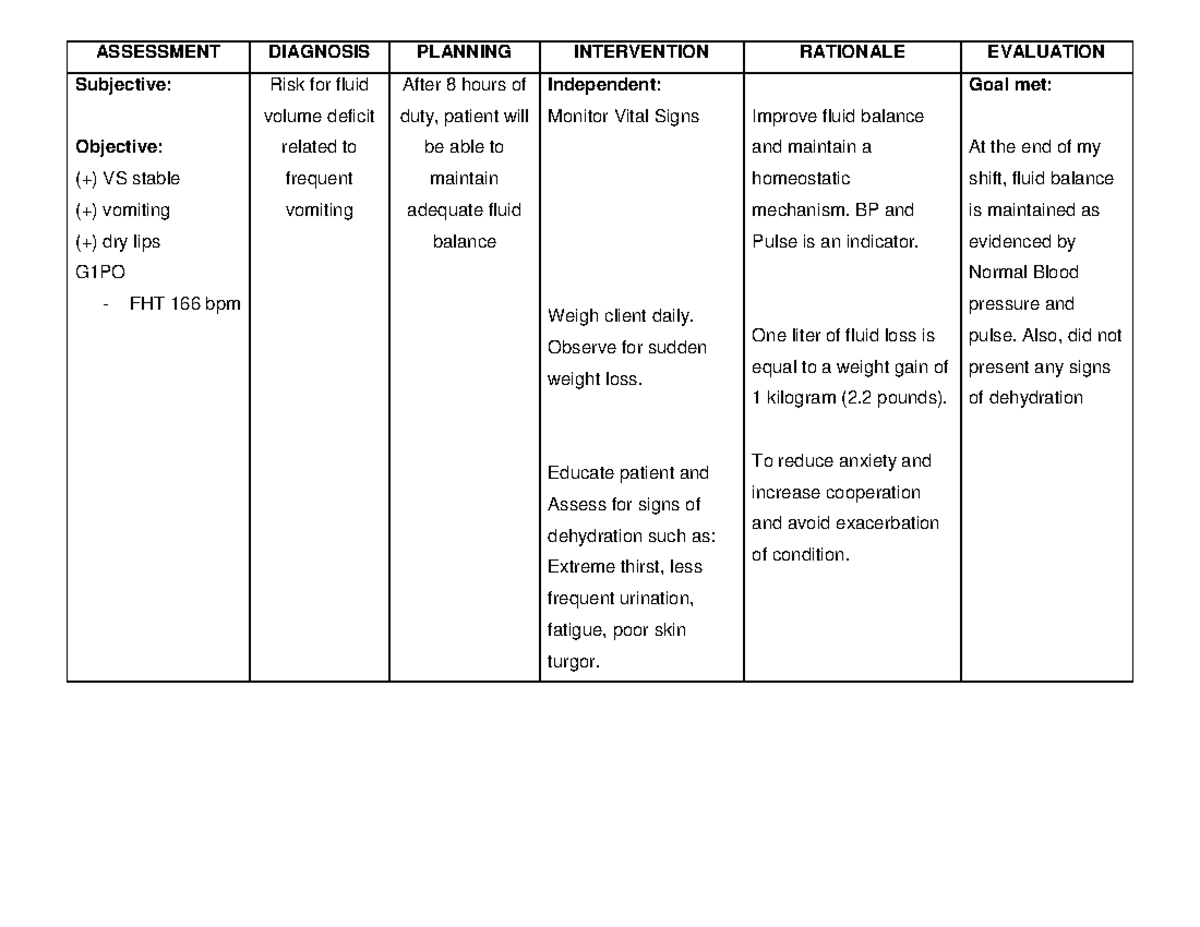
Image: www.studocu.com
Laboratory Tests and Monitoring
In addition to physical assessment, laboratory tests are valuable for confirming fluid volume deficit and monitoring its progression. These tests may include:
- Electrolyte Levels: Dehydration can cause imbalances in electrolytes such as sodium, potassium, and chloride.
- Hemoglobin and Hematocrit: These tests can help determine blood concentration, which may be elevated in dehydration.
- Urine Specific Gravity: A high specific gravity suggests concentrated urine, indicating dehydration.
Develop a Nursing Care Plan for Fluid Volume Deficit
Once a risk for fluid volume deficit has been identified, it’s crucial to create a tailored nursing care plan. This plan should outline the specific interventions required to prevent or manage the condition. It’s essential to assess each patient’s individual needs to create the most effective plan.
Nursing Interventions to Prevent and Manage Fluid Volume Deficit
The key focus for interventions is to address the underlying causes of dehydration while promoting adequate fluid intake. Some common interventions include:
- Fluid Therapy:
- Oral Rehydration: Encourage patients to drink plenty of fluids, such as water, clear broth, or electrolyte solutions.
- Intravenous (IV) Fluids: If oral hydration is not possible or insufficient, IV fluids may be necessary to quickly restore hydration.
- Monitor Intake and Output: Accurately record fluid intake and output to ensure the patient is receiving and eliminating enough fluids.
- Assess Vital Signs: Regularly monitor vital signs like heart rate, blood pressure, and temperature.
- Educate Patient and Family: Educate patients and their families on the importance of adequate fluid intake, early signs of dehydration, and how to manage the condition at home.
Tips and Expert Advice to Enhance Fluid Volume Deficit Management
Effective management of fluid volume deficit requires a combination of preventive measures and proactive interventions. As a nurse, I’ve learned the importance of these key tips:
- Proactive Approach: Don’t wait for symptoms to appear. Implement preventive measures, especially for patients at high risk of dehydration.
- Individualized Care: Remember that everyone’s needs are different. Tailor your care plan to each individual’s risk factors and preferences.
- Communication is Key: Collaborate with other healthcare professionals, including physicians, pharmacists, and nutritionists, to ensure a unified approach to fluid management.
- Patient Empowerment: Teach patients and their families about the importance of staying hydrated. Encourage them to take an active role in their own care.
Frequently Asked Questions (FAQs)
1. What are some common signs of dehydration in children?
In addition to the signs mentioned above, children may show signs such as sunken fontanels (the soft spots on a baby’s head), dry diaper, and fussiness. If you suspect a child is dehydrated, it’s important to seek medical attention immediately.
2. How much fluid should I drink per day?
The amount of fluid needed varies depending on age, activity level, and climate. However, a general guideline is to drink about eight glasses of water per day.
3. How can I prevent dehydration during exercise?
Drink plenty of fluids before, during, and after exercise. Choose sports drinks containing electrolytes to replenish minerals lost through sweat. Listen to your body and slow down or stop exercising if you feel thirsty or lightheaded.
Risk For Fluid Volume Deficit Ncp
Conclusion
Understanding the nursing care plan for fluid volume deficit is crucial for every nurse. Being able to efficiently assess, prevent, and manage this condition is essential for the well-being of our patients. By emphasizing preventive measures, closely monitoring our patients, and tailoring interventions to their individual needs, we can successfully address this common health concern.
Are you interested in learning more about fluid volume deficit management? Share your thoughts in the comments below!





